By Arnold Linga
Taita Taveta County, Kenya: When *Jane quietly walked into the small softly-lit counseling room at one edge of the Mwatate sub-county hospital on a late afternoon, her tentative smile concealed the great burden she had been carrying inside for months.
The only sign that all was not well was the troubled shadow that lurked deep in her.
Her first words had a solid tone of finality.
“I am tired.”
Then the floodgates opened. The deep anxiety, unending uncertainties, and unspoken frustrations that had festered inside her for ages had finally found a vent. Words tumbled out. Tears came. Sniffles followed.
At 28, her life had ground to a halt. Her teaching job had been terminated after the closure of schools.
Following the outbreak of Covid-19. At her home, tension was rising between her and her husband. For people used to the morning ritual of waking up and leaving for work, this new normal of waking up and idling in the house the whole day was straining their marriage.
Ms. Rebbeca Macharia, a clinical psychologist at Mwatate Sub-County Hospital, says that the woman whom she only refers to as a special client was in a suicidal state.
“We started and had several sessions with her. We talked about everything and anything; family and her decisions. When she said she would keep coming back, it was a breakthrough because the process of healing had started,” recalls the medic.
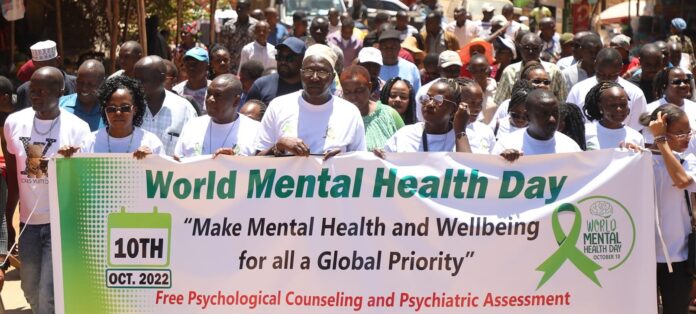
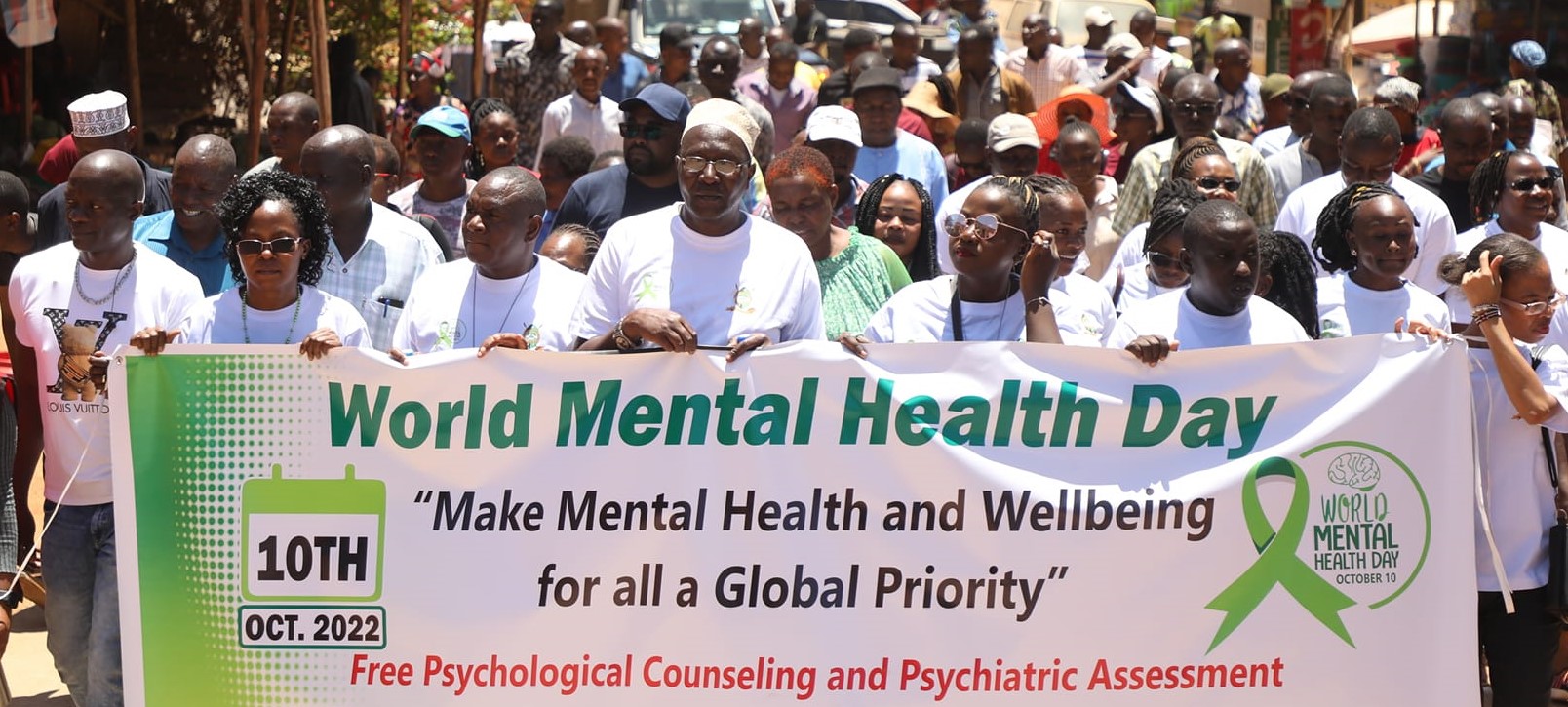
Mental health issues in Taita-Taveta County have been a major cause of concern for health experts largely, especially after a sharp surge in cases reported following the covid-19 pandemic.
What makes the situation more precarious is the fact that most mental health issues are either associated with witchcraft, curses, or bad omens which forces the victims of mental problems to seek help from spiritual healers, pastors, or traditional medicine men.
Ms. Eva Mwadembo, the County Mental Health and Gender-Based Violence (GBV) Coordinator, says mental health issues have become a silent pandemic that is sweeping across the region yet the underlying issues contributing to those conditions remain largely unaddressed.
Data from the health facilities paint a bleak picture of mental health issues in the region. In the post-Covid 19 eras of 2021, a total of 2,152 cases were reported in health facilities across the county. These cases include conditions such as depression, schizophrenia, and psychosis amongst others. In 2022, the data shows that reported cases of mental health surged higher to 3,174 with more cases expected to grow exponentially as the community becomes more enlightened on mental issues.
Ms. Macharia says coordinated efforts at the facility level and the introduction of novel ideas on how the issue of mental health can be introduced at a typical community set up at the peak of COVID-19 has significantly contributed to demystifying such disorders. Such ideas include community outreach sessions where psychologists give a talk to the community away from hospitals.
She adds that constant engagement with key leaders in the community including school heads and church leaders through targeted outreach programs has also contributed to increasing the understanding of mental disorders and lowering the stigma associated with mental health challenges.
“We have liaised with religious leaders where families take kin with mental challenges for prayers. After prayers, the church leaders often refer the cases to hospitals for specialized treatment. This partnership has helped patients who need medical treatment to come to hospitals to get help” she explains.
Rev. David Zowe, head of House of Prayers; a church at the populous Sikujua village in Voi sub-county, says the religious leaders offer prayers to deal with rare incidences of genuine spiritual possessions. However, when they determine that mental health cases are medical, they send the patients to health facilities for help.
The cleric added that the effects of mental health disorders on the community’s well-being are getting prominence with such issues being discussed at the pulpit.
“These are issues that we are talking about at the pulpit. We are also inviting professional counselors and psychologists to come to address the congregation as part of creating awareness on this topic rarely talked about,” he noted.
One of the major challenges facing efforts to address mental disorders in the region is the absence of a framework to combat the issue. In most health programs, mental issues are treated as a small component rather than being viewed as a serious matter requiring specific attention. This is despite the Ministry of Health found that one out of every four people seeking health services suffers from a mental disorder.
Ms. Macharia adds that low budgetary allocation and the absence of a robust funding program to extend the mental health wellness programs to marginalized areas remain a challenge to tackling such issues.
She further points out that ailments like high blood pressure and ulcers amongst young people can be outcomes of long periods of stress due to coping with life challenges. She argues that addressing stress-related issues can lead to a reduction of such issues.
“We have cases of fairly young people suffering from body ailments that arise from mental distress. Treating mental issues can stop such ailments,” she says.
Dorah Mkakisha, a forty-year-old grandmother from Kishushe in the Taita sub-county says her lower-primary school grandchild was clinically diagnosed with acute depression in 2020 and prompt medical interventions have seen the youngster recover and he currently works as a security guard in Mombasa while pursuing a course in welding.
“My grandchild got early help and he defeated the illness. He completed his primary school education and now works as a security guard in Mombasa while taking evening classes for a welding course,” said Mkakina.
The silver lining of it all is the successful change in perception about mental health. The local communities are now moving away from the belief that mental disorders are caused by sorcery, demons, and other traditional phenomena.
As per recent mental health data, it is clear that more people and families are now seeking medical attention for mental health issues as awareness spreads and a shift in belief takes shape.
This publication was produced with the financial support of the European Union. Its contents are the sole responsibility of Arnold Linga and do not necessarily reflect the views of the European Union.