By Sharon Kiburi
Nairobi, Kenya: HIV remains one of the greatest pandemics affecting human lives, experts warn that the government and people have let their guard down which is increasing infections.
Speaking during the 41st science café held by Media for Environment, Science, Health & Agriculture (MESHA). Dr. Jonah Onentiah, HTS Program Manager at the National AIDS and STIs Control Programme (NASCOP), said even though the country was experiencing an increase in the number of people using self-test kits, more still needs to be done.
He said their experience at NASCOP has shown that many Kenyans still do not know their HIV status because of stigmatization.
“HIV self-testing (HIVST) is a process in which a person collects their own sample (oral fluid or blood), performs an HIV test, and interprets the result. It is often done in private or either alone or with someone trusted,” said Dr. Onentiah.
Dr. Onentiah said the self-test does not provide a definitive HIV-positive diagnosis, and all reactive (positive) self-test results need to be confirmed by a trained health provider using the national testing algorithm.
Innovative technology has allowed the development of self-testing that creates provision for privacy, autonomy, confidentiality, testing at own comfort, and whether to use blood samples or oral silver fluid.
Using the HIV self-testing, Speaking with Josephine Awinja, “ “I have used Insti HIV kit and Alere HIV-1/2, the instructions were so simple and direct to what is required. I took the test, but it was so scary since I had to prick myself alone; I wasn’t sure what the result would be. I had several questions in my mind due to tension that made me check on the result after so many hours. But all in all, after checking on the result immediately, I did another test with more courage now to confirm the first result” she explains.
While Christopher Kimotho, a medical officer, said, “I used the rapid HIV test (blood), using the kit was not difficult to follow. The experience was confidential and a calm one.
“When I heard about these self-testing kits, I was curious and walked into a pharmacy to get my hands on a kit. I was pleasantly surprised to find out that the chemist not only had the kits but there were options,” said Fred Otieno. However, despite having been given the instructions by pharmacists about using the kit, Otieno says he was unsuccessful in taking the test.
“ I tried pricking myself. I must have done it wrong since no blood came out; I threw away the testing kit. I think I will give it another try soon,” said Otieno.
This was in a bid to beat the constraints associated with traditional HIV testing, such as stigma, provider’s attitudes, long waiting periods, having to travel long distances, inadequate staffing, and facilities operating for scant hours.
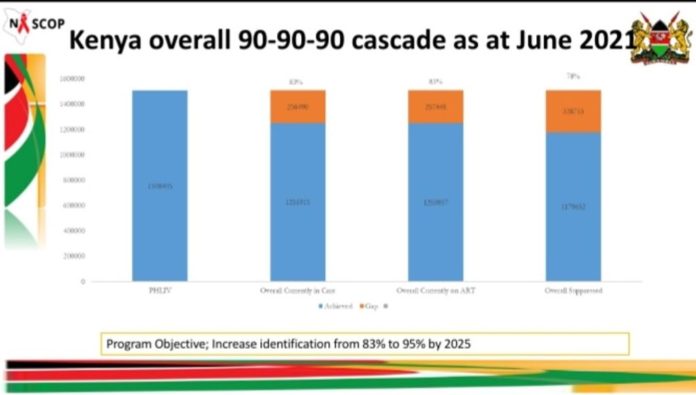
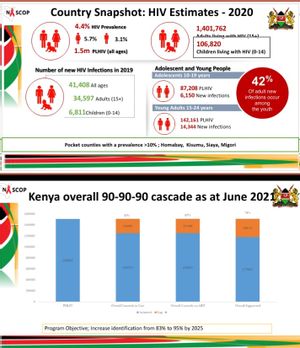
As of September 2021, Kenya has four nationally approved HIV self-testing kits–Ora Quick, INSTI, Sure Check, and Atomo. According to NASCOP Kenya, a country snapshot, adults living with HIV age fifteen plus are 1, 401,762 while the number of children living with HIV is 106,820. HIV prevalence in the country is at 4.4.% percent, of 1.5 Million people among people of all ages. Moreover, 42% percent of new infections occur among the youth.
As Kenya launched the undetectable equal untransmittable (U=U) campaign on September 14th, 2021, it was noted that HIV self-testing would play an integral role in ensuring the campaign’s success.
“The success of the U=U campaign will be effective if the HIV-infected individuals are identified and put on Highly active antiretroviral therapy treatment (HAART), maintained compliance, and durably maintain an undetectable viral load (below 50 copies),” said Dr. Peter Mogere, a primary healthcare advocate and HIV prevention enthusiast.
“HIV self-testing is very integral in playing a part of U=U. It will be utilized to diagnose individuals infected with HIV, who may then be put on Highly active antiretroviral therapy. With good adherence, suppressed viral load will be achieved.”

Dr Mogere says HIV self-testing vending machines will ensure the kits are available at any time at specific places. Vending machines provide anonymity, which enhances confidentiality.
The vending machines may not increase awareness of HIV; however, they may increase HIV testing by targeting individuals with challenges of visiting health facilities, pharmacies, or picking the kits from the community.
Dr. Mogere says that for the effectiveness of HIV vending machines to be realized, the government and implementing partners (including the media) must create awareness.
“The approved test kits come with package inserts in English and Swahili with a step-by-step pictorial demonstration of how to conduct the self-test. However, if someone is illiterate, they may need the help of the clinical health personnel or the person delivering the self-test kit.,” said Dr. Mogere.
Onesmus Kamau, the head of the e-Health and Systems Development Unit at the Ministry of Health, says efforts are being made to ensure HIV self-testing reaches the entire population by including a visual demonstration of how the kit is used; recorded in vernacular for the different tribes in Kenya.
As of 2019, Kenya had 1.5 million people living with HIV. Of the number, 4.5 percent were adults ages 15 to 49. That year, there were 42000 new HIV infections and 21,000 AIDS-related deaths. In the same year, 75 percent of adults and 63 percent of children were on antiretroviral treatment, as reported by UNAIDS in 2020.
Further, Kenya has the joint third-largest epidemic globally, alongside Mozambique and Uganda, according to global information and education reports on HIV and AIDS. The report further shows that Kenya’s HIV epidemic affects most of its general population, but Key populations are still more vulnerable to infection.