By Clifford Akumu
Siaya County, Kenya: On a chilly Monday morning, tens of pregnant women, girls, and breastfeeding mothers went to Randago Dispensary in Alego-Usonga, Siaya County, for their routine clinic visits to receive medical attention.
Their gaze was occasionally interrupted by the steady flow of patients to the facility and the constant movement of healthcare professionals and promoters brandishing medical paraphernalia.
At the pediatric section, I met Veronica Akinyi, who was going through a list of names on a hard-cover booklet inscribed ‘PMTCT Appointment Diary.’ Occasionally, she would counter-check with the facility’s digital patient management system on her hand-held tablet to see who had missed their appointment.
Akinyi followed up with phone calls to find out why some mothers on her list did not report to the facility. In cases where she did not get a response, she would conduct home visits. Akinyi has been passionate about this for the last seven years.
She is racing against time to close the mother-to-child HIV transmission gap that statistics show is increasing every day. According to the Joint United Nations Programme on HIV/AIDS (UNAIDS), 1.2 million children and adolescents living with HIV (0-19 years) in the world are untreated.

The National Syndemic Diseases Control Council (NSDCC) 2023 HIV Estimates indicate that Kenya managed to reduce new HIV infections by 57 percent and AIDS-related deaths by 68 percent in 2023 compared to 2022.
The agency further notes that Kenya fell short of meeting the target to reduce mother-to-child HIV transmission rates to less than five percent by 2020.
The current national HIV mother-to-child transmission stood at 8.6 percent as of 2022. This means nine in every 100 HIV-positive mothers transmit HIV to their children during pregnancy, labor, and delivery or while breastfeeding. Treatment coverage for children living with HIV is 85 percent, with about 74 percent of those on treatment virally suppressed.
“Children have been left behind, and their voices unheard.”
Akinyi is part of a growing network of mentor mothers who can often recite from memory the names of clients and locations of clinics throughout the region that offer HIV prevention, treatment, and care services for women and girls living with the disease.
Role of Mentor Mothers
Mentor mothers are mothers living with HIV who have been trained to provide adherence and psycho-social support to pregnant and breastfeeding persons living with HIV to protect their babies from infection. They also trace women who interrupt treatment and provide health education.
In 2007, when Akinyi learned about her HIV status during her first visit to the ante-natal clinic, she vehemently contested the results. In her mind, she thought maybe the testing machines were faulty. She even considered a second opinion but lacked the courage to take that approach. She made her maiden ANC visit while seven months pregnant.
“ I had never even cheated in my new marriage,” said Akinyi. “How was my husband going to react? How would we live in the same house with all the guilt?”
Still in denial, Akinyi refused to be put on anti-retroviral medication. She later attended the second ANC clinic and got tested, and I still received the same results. The doctors advised her to bring the husband to the clinic so that they could be tested as a couple, but the husband became violent, noting he was very okay and there was no need to conduct the test.
She stayed without taking anti-retroviral medication until she gave birth in December 2007
Even though she picked up the medicine from the facility, she ensured none reached home. She threw them away along the way.
By 2009, she was carrying her second child. “I knew I had HIV/AIDS, but insisted I get retested since I had little faith in the previous tests,” she continued. And just like her first pregnancy, she would later give birth to her second child without taking medication. All this while she was worried her children might have contracted the virus.
Luckily, both children turned out to be HIV-negative. Akinyi never revealed her status to her husband since the husband never wanted to get tested.
In 2010, her husband became very sick. He was tested and found to be HIV positive. And when I was also tested, it turned out to be positive. On top of being HIV positive, her husband was also diagnosed with tuberculosis. By October of the same year, he died.
That same month, she started her medication. She was put on Septrin medication until 2012 when she was fully enrolled in ARVs. Septrin is a combination antibiotic primarily used to treat certain bacterial infections, including pneumonia and bronchitis. Akinyi took septrin to treat recurring bacterial infections.
In 2012, Kenya adopted the Mentor Mother Model as a national policy as one of the core strategies for the elimination of mother-to-child transmission of HIV and syphilis (2016-2021).
Consequently, when the Ministry of Health’s Mentor Mother Program came calling, Akinyi was lucky to be part of the team. She got attached to Randago Dispensary (which provides holistic and accessible HIV and Tuberculosis care and treatment services). In 2018, the Ministry of Health agreed with The Global Fund to expand the mentor mother program further into all 47 counties of Kenya.
The Program, centered on engaging women peers living with HIV in communities, addresses gaps in the prevention of mother-to-child transmission of HIV by providing maternal, newborn, and child health services. It empowers women peers to share their lived experiences to support newly diagnosed HIV-positive pregnant and breastfeeding women and their children, contributing to the goal of ending AIDS in children.
Akinyi plays a critical role in global health security. As a mentor mother, she is the first contact with pregnant mothers and teenagers before they see the doctors for medication.
Because of mentor mothers like Akinyi, the communities understand the importance of giving birth to HIV-free babies, and they don’t hesitate to be enrolled in treatment.
“We serve as the link between the community and health facilities,” Akinyi shared.
She recalls her first encounter as a mentor mother: “I was afraid at first but later gained the courage and energy. It makes it very easy to teach the mothers. Every time you are tested and found to be positive, it’s good to start treatment immediately.
“We encourage women to bring their spouse to the clinic for their next check-up and explain that we won’t reveal their status but talk them through the plan to test them for HIV as a couple,” she revealed.
Back at the dispensary, Akinyi has already gathered a small group of women under a Jacaranda tree for a psycho-social support group session before the PMTCT mothers proceed to see the nurse. She attends to 64 mothers and young girls in the clinic (58 breastfeeding and six pregnant clients). Pregnant mothers attend clinics on Tuesdays, lactating mothers on Wednesdays, and pregnant teenagers on Fridays.
When the mothers visit the dispensary for their routine visit, they meet with the mentor mother first –who is always at the facility when not on a home visit – before seeing a clinician or nurse.
“When they come to the facility, we take about one hour to share stories on how they are doing and reacting to the treatment. After that, we do the weighing before they proceed to be attended to by the nurse,” she explained. She further added that any issues that emerge from these sessions are reported to the clinician or nurse on duty for action as they may interfere with treatment outcomes.
Immediately after the psycho-social group meeting, Akinyi informed me that one of her regular clients had not reported and was not picking up her calls. Because I wanted to get a feel for the tracing process, we embarked on a one-kilometer trek to Ulowa village to look for her.
We found Joan Atieno* preparing breakfast for her eight children (five boys and three girls). The sight of cassava and potatoes in the small pot boiling in a three-stoned fireplace. The worn bedding spread at the compound’s entrance illustrated the poverty level.
“We have no food. Look at what I managed to get from the farm. They are not even mature, but I have no choice,” she said, pointing at the boiling pot.
Atieno, 38, a peer mentor mother program beneficiary, confirmed that the program had been eye-opening and saved her children.
“I look at my children with so much pride. It’s like life gave me a second chance through them. I owe all these to the mentor mother program,” she narrated.
She met Akinyi in 2018 when she regularly visited the dispensary after being sick for several weeks. Atieno explained that she started experiencing unusual health problems. Alarmed, she decided to get tested for HIV.
“ I was diagnosed with HIV. I felt a mixture of fear, shock, and regret. Since that day, my relationship with my husband has been strained. We sometimes have small differences, but we solve them ultimately,” said Joan.
Atieno remembered how Veronica and the doctors at Randago Dispensary, where she receives her antenatal care, were of help. She took every bit of advice from Akinyi and the doctors and never missed taking the ARV pills. The prescribed drugs helped her prevent transmission of the virus to her children.
Emily Nabwala, a clinical officer in charge of the Comprehensive Care Clinic at Randago Dispensary, said mentoring mothers’ work has improved the facility’s prevention of mother-to-child transmission.
“In our PMTCT program, we are recording over 96 percent of the mothers who are virally suppressed- meaning they have achieved and maintained a low viral load of HIV in their body. We only have one pregnant mother whose viral load is above 1,000 and a few breastfeeding mothers who have low-level viremia. (simply HIV-1 plasma viral load above the limit of quantification of clinical assays, usually between 20-500 copies/mL).”
These lower viral loads are associated with better clinical outcomes and slowed disease progression, as well as reduced HIV incidence in the community, Nabwala added.
She added that the viral suppression rate in the general population that attends the facility ” is unfortunately not as great as we would want it to be. Currently, we have a viral suppression rate of around 70 percent in the general population.”
Nabwala noted that mentorship has had an impact on stigma reduction, honoring clinic appointments, and viral suppression as a result of consistent health talks regarding medication.
Dr. Patrick Oyaro, Chief of Party, USAID Stawisha Pwani project and a champion of Paediatric HIV, also highlighted the remarkable progress in pediatric HIV medication.
“We started with antiretroviral medications such as zidovudine (AZT) and Nevirapine that were being used in the treatment and prevention of HIV, but over time, having a parent administer or measure some of these drugs accurately would be a challenge because of a lack of education or time to take the proper measurements. Then came dolutegravir, which is easily tolerated and has contributed to the reduction of mother-to-child transmission,” Dr. Oyaro said.
It is vital to make sure the parents help the children adhere to treatment- so that they get viral suppression and do not develop any resistance, he noted.
Joan Atieno emphasizes that her daughter had to take the syrup for a year and a half, something she was very keen on. Two years later, her two-year-old daughter is HIV-negative and healthy.
Patricia Jeckonia, Senior Technical Advisor at LVCT Health, says some of the reasons MTCT rates are still high are women not attending antenatal clinics, the knowledge gap amongst providers, and the lack of testing kits. However, another major cause is the lack of HIV retesting throughout the pregnancy.
“Majority of women are tested at the start. Very few of them get to be tested in the third trimester or even during labor since most hospitals don’t have enough test kits. They get the subsequent testing, maybe six weeks, which is also not guaranteed. This doesn’t seem right because the virus cannot be detected early enough without retesting,” she asserted.
Early detection is crucial for initiating timely interventions and treatments to reduce the risk of transmission to the fetus. Available data show that without treatment, one in four babies will get HIV infection from their mother, but with treatment, the chance of infection is as low as one in 100.
Several countries, including Kenya, made a declaration to end HIV in children by 2030. However, Kenya has chosen to accelerate its target by three years, aiming to achieve this goal by 2027.
The “Kenya Plan to End Aids in Children by 2027” initiative hopes to reduce the rate of MTCT of HIV from 8.6 percent to below five percent and to increase and sustain treatment coverage and HIV viral load suppression among pregnant and breastfeeding women, children, and adolescents living with HIV to not less than 95 percent.
Dr. Ruth Laibon-Masha, Chief Executive Officer of the National Syndemic Disease Control Council stressed the need to aggressively address the challenge of breastfeeding mothers, and HIV transmission between father, mother, and mother-to-child.
“We have a large cohort of women who come to the facility to deliver and test negative. They go back home and, due to cultural practices, they go back to their untested husbands. There is a need to design programs to put men at the center of efforts to eliminate mother-to-child HIV transmission,” said Dr. Laibon-Masha.
Zipper Imbuye, Head of PMTCT Siaya County and Family Planning, explains achieving. an HIV-free generation in the county hinges mainly on the success of preventing mother-to-child HIV transmission.
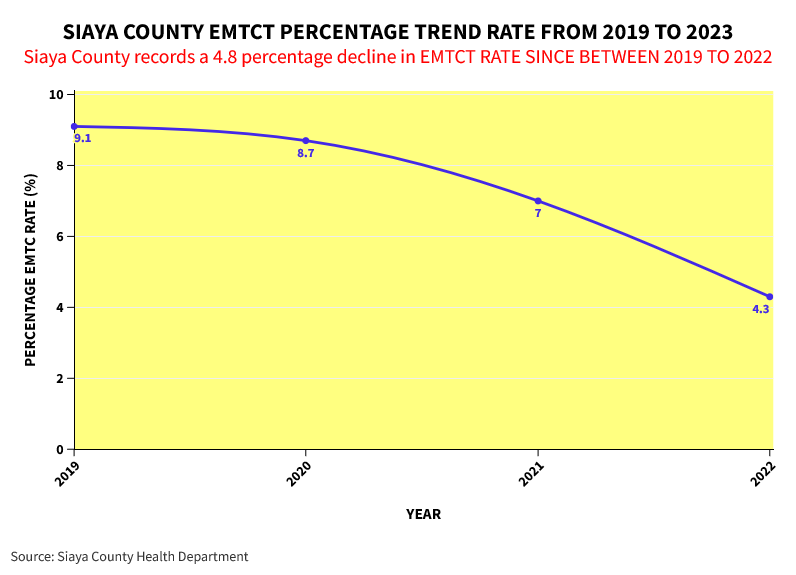
With a 4.3% PMTCT rate, Siaya County demonstrates the impact of multi-thronged interventions in child HIV response. Why has the initiative worked well in Siaya County?

“We owe this achievement to the clients, mentor mothers, and the community. It has been a long struggle. We endeavor to sustain the gains so the WHO can accredit us,” Zilper explained.
According to the National HIV Estimates, Siaya County had a PMTCT rate of 21 percent in 2015, 12.2 percent in 2016, and 8.7 percent in 2020 to the current estimates of 4.3 percent in 2022.
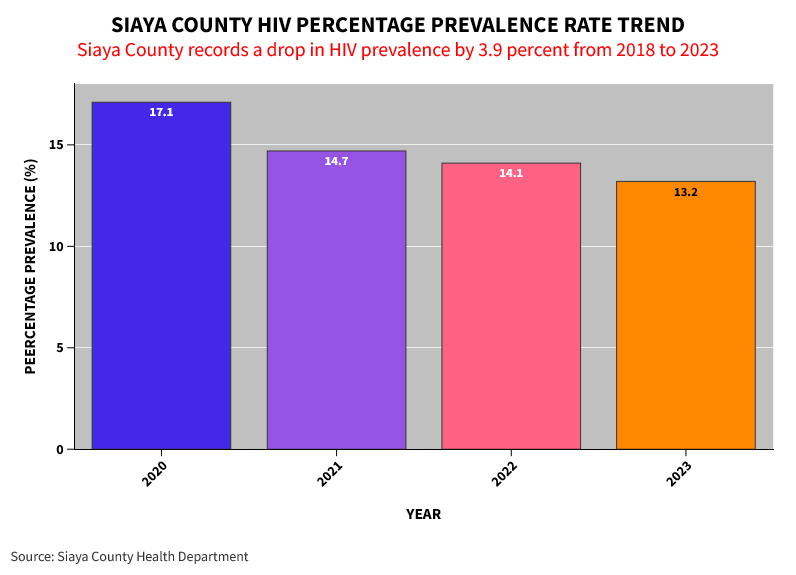
The County, Imbuye adds that it has adopted an integrated approach in its quest to end HIV transmission to babies. “As a county, we are working together with partners, adolescents and young people, peer educators, the fisherfolk, discordant couples, and critical populations like those who work in gold mines to design and roll out programs and interventions toward the reduction of mother-to-child transmission,” intimated Imbuye.
Another critical limitation of the mentor mother program, noted Akinyi, is the high poverty levels. “Some of the women who visit the hospital have high viral loads because they do not take medication when they have no food. I advise them to drink warm water before taking their medication,” Akinyi shared.














